Caregiver Connections
Helpful tips for family caregivers
July/August 2020
Even before COVID-19, many older adults experienced loneliness and isolation. Fortunately, the pandemic has brought new ideas, and revived old ones, to help families support their solo seniors. In our second article, we describe what a full dementia workup involves. Although Alzheimer’s is the most common memory loss condition, there are many others. It’s important to formally determine a diagnosis, because some conditions actually do have a cure. Last, we complete our series about osteoporosis, with suggestions for food and exercise habits that can strengthen bones and slow bone loss.
Share Page:
The importance of staying connected
 Staying connected is extremely important.
Staying connected is extremely important.
Isolation and loneliness are not just sad situations. They have been shown to increase the likelihood of dementia, depression, and heart disease in older adults. Even early death. As a family caregiver, you may be struggling to find ways to have meaningful interactions. Especially if the person you care for has dementia.
Below are some ideas to boost connection. Some require technology. Others do not.
- Video calls. Video calls top the list in terms of reducing isolation and loneliness. Studies show that video chatting results in half the depression experienced by those who use only email, social networks, or instant messaging.
- Old-fashioned snail mail. Your relative’s generation is used to writing and receiving letters. Consider buying postcards (flowers, baseball stars, etc.) to make it easy to pop a note in the mail. Unlike phone calls, cards can be displayed as a visual reminder of love sent and received.
- Telephone calls with an activity. Consider doing the day’s crossword puzzle together. Or agree to read a book together or watch a show you can both discuss.
- Explore reminiscence activities. Begin with casual questions now and then about the past. (Tell me about your wedding day. Your first job …). Even if you’ve heard the stories before, encourage more detail. Check out the StoryCorps Connect project at the American Folk Life Center of the Library of Congress. This new program enables a family member to record and store a 40-minute interview using video conferencing technology.
- Consider a telephone check-in service. Many people are volunteering to call isolated seniors. They have been trained to be good listeners and to spot signs of trouble. Check the local senior center to see if they have a phone check-in program. Or contact Covia Social Calls. This free service provides nationwide telephone check-ins by trained volunteers.
What's in an Alzheimer's test?
 When symptoms of memory loss or confused thinking arise, it’s natural to wonder: Is it Alzheimer’s?
When symptoms of memory loss or confused thinking arise, it’s natural to wonder: Is it Alzheimer’s?
There is no specific test for Alzheimer’s disease. To achieve a diagnosis, doctors typically order a variety of tests.
Most of the tests are to rule out the many, many conditions besides Alzheimer’s that can cause similar symptoms. Some of these have cures. Some do not.
A primary physician is likely to order three types of tests:
- A medical exam with lab work. The doctor will review your loved one’s medications and take a thorough family history. Blood and urine tests will check for problems with the thyroid, liver, and kidneys. Your relative also will be asked to outline what symptoms began and when, and to answer questions about alcohol and drug use and other lifestyle habits. (You may be asked to attend this session.)
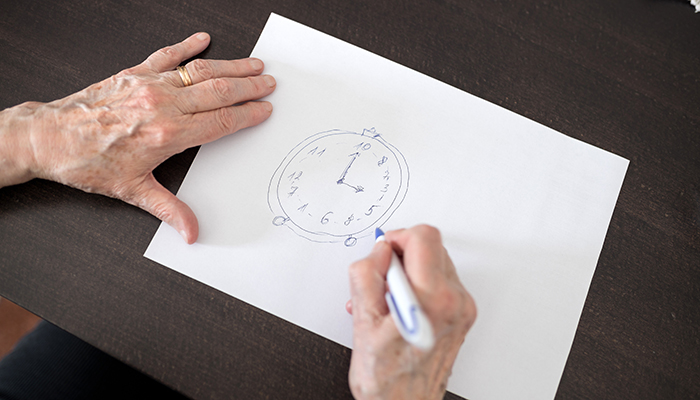
- A neuropsychological evaluation. This is a series of tests involving word questions, drawing, and puzzles. The tests assess the functioning of different parts of the brain to discern where there are impairments: Are there problems with memory? With the ability to plan? With language? With math? With judgment? Additional survey questions help rule out depression or other mood disorders that cloud thinking.
- Brain imaging. A CT and/or MRI scan can detect signs of a tumor, stroke, or head injury. A PET scan highlights parts of the brain that have less activity than others.
Once the results are in, your family member can meet with the primary physician to review the findings. Again, the doctor is likely to want you to be present. (Your relative may need help following the discussion. Also analyzing the pros and cons of recommended treatments.)
There is no cure for Alzheimer’s itself. But the sooner you have a diagnosis, the sooner you can act. With treatment if it’s one of the curable dementias. Or medication to slow the progression of an untreatable condition. An early diagnosis also gives you time to make plans for the future.
Return to topOsteoporosis: What you can do
 If you are concerned about a loved one’s osteoporosis—brittle bones—it’s a good idea to bring this up with the doctor. He or she will likely discuss various medicines that can help.
If you are concerned about a loved one’s osteoporosis—brittle bones—it’s a good idea to bring this up with the doctor. He or she will likely discuss various medicines that can help.
In addition, changes in daily life outlined below can go a long way to making stronger bones. Consider:
Calcium. The best food sources are low-fat dairy products; dark green leafy vegetables; canned salmon, mackerel, or sardines (with bones); and tofu. Women over age 50 should consume a total of 1200 mg of calcium per day. Men need 1000 mg/day until age 70. Then they too should get 1200 mg/day. A supplement is fine. But be sure to pick a dose that factors in the calcium your relative already receives from food. More than 2000 mg/day may increase the risk of heart disease and kidney stones.
Vitamin D. Exposure to sunshine yields vitamin D. But only when sunscreen is not used (no free lunch!). Look for foods such as milk that have been fortified with vitamin D. Or get a supplement. Adults age 51–70 are advised to take 600 international units (iu)/day. Those over age 71 need 800 iu/day. African Americans don’t absorb vitamin D well through the skin, so 2000 iu is the recommended supplement. Most people can safely take up to 4000 iu/day.
Strength exercises. Weight-bearing exercise works with gravity to produce strong bones: Brisk walks, hiking, dancing, climbing up stairs. Resistance training also helps: Lifting weights or using exercise bands. Talk to the doctor about the safest way to build up strength.
Lifestyle changes
- Get up off the couch! A sedentary lifestyle leads to brittle bones.
- Limit alcohol to no more than two drinks/day. Alcohol kills bone cells and leaches calcium from the bones.
- Stop smoking. Smokers’ bones heal more slowly.

